Global Health
Understanding the transjugular intrahepatic portosystemic shunt (TIPS) procedure.
I had cared for several patients who had transjugular intrahepatic portosystemic shunt (TIPS) surgery, but I didn’t really know what it was. If you are a nurse caring for patients after TIPS placement, here’s what you need to know.
AND
Liver anatomy
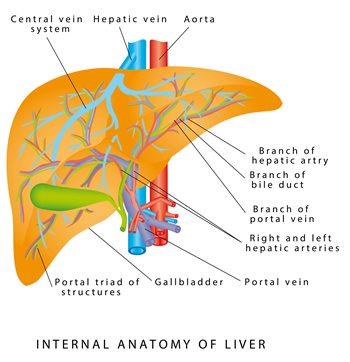 Let’s start with an overview of the basic anatomy of the liver. The portal vein transports blood from the stomach, intestines, spleen, gallbladder and pancreas to the liver. In the liver, blood flows through capillaries, where old red blood cells, bacteria and other toxins are filtered out and nutrients are added. The blood then leaves the liver back into the circulation via the hepatic veins. This system of vessels is called the portal vein system.
Let’s start with an overview of the basic anatomy of the liver. The portal vein transports blood from the stomach, intestines, spleen, gallbladder and pancreas to the liver. In the liver, blood flows through capillaries, where old red blood cells, bacteria and other toxins are filtered out and nutrients are added. The blood then leaves the liver back into the circulation via the hepatic veins. This system of vessels is called the portal vein system.
Diseases such as hepatitis, fatty liver disease, and excessive alcohol consumption damage the liver, leading to scarring or cirrhosis, which can block vessels in the liver, preventing proper blood flow. When blood cannot leave the liver properly, it backs up, increasing pressure throughout the network; this is called portal hypertension. High pressure can cause ascites and varicose veins in the esophagus, duodenum, rectum or umbilical area. Other causes of portal hypertension include blood clots in the portal vein, parasitic infection (schistosomiasis), and focal nodular hyperplasia. The TIPS procedure reduces portal pressure by creating a channel between the hepatic vein and the intrahepatic branch of the portal vein.
AND
Indications TIPS (Bajaj, Sanyal and Collares, 2023)
The TIPS procedure is indicated in the following cases:
- Esophageal varices:
- Control active bleeding varices that fail to achieve first-line hemostasis or cause rebleeding within 120 hours of initial hemorrhage
- Prevent recurrent bleeding
- Stomach varicose veins
- Ectopic varicose veins (duodenum, rectum, peristomy)
- Portal hypertensive gastropathy (changes in the gastric mucosa)
- Refractory ascites: (ascites that does not respond to medical treatment)
- Budd-Chiari syndrome (hepatic veins blocked or narrowed by a clot)
- Liver pleural odor: (pleural effusion (>500 ml) in a patient with cirrhosis)
- Bridge to liver transplant
GUIDELINES Contraindications (Bajaj, Sanyal and Collares, 2023)
| Congestive heart failure | Liver tumors |
| Severe tricuspid regurgitation | Obstruction of all hepatic veins |
| Severe pulmonary hypertension | Hepatic encephalopathy |
| Polycystic liver disease | Portal vein thrombosis |
| Active systemic infection or sepsis | Thrombocytopenia |
| Untreated biliary obstruction | Moderate pulmonary hypertension |
Testing the Pre-TIPS Procedure (Bajaj, Sanyal, & Collares, 2023)
The following tests are performed before TIPS is placed:
- Complete blood count
- Total bilirubin
- International Normalized Ratio (INR)
- Serum creatinine
- Model for end-stage liver disease (MELD) scoring.
- Liver imaging, such as contrast-enhanced computed tomography (CT), magnetic resonance imaging (MRI), or noncontrast abdominal ultrasound with Doppler
- Chest X-ray to evaluate for fluid overload and cardiomegaly
- Complete cardiac evaluation in selected patients with signs, symptoms or history of heart failure, tricuspid regurgitation, cardiomyopathy or pulmonary hypertension
TIPS Procedure (Bajaj, Sanyal, & Collares, 2023; Lippincott Procedures, 2023)
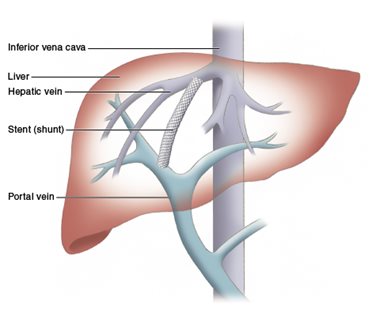 TIPS is a minimally invasive procedure performed in the interventional radiology department by specially trained staff, but understanding the procedure is useful for anyone educating patients or providing pre- and post-procedure care. Sedatives and/or painkillers will be administered. During fluoroscopy, a catheter is typically inserted into the right jugular vein and advanced down the superior vena cava into the right or middle hepatic vein. There, the contrast is used to identify the internal hepatic circulation. The TIPS needle is then inserted through the hepatic vein catheter into the portal vein. A stent is placed, connecting two veins to create a shunt, which reduces portal pressure.
TIPS is a minimally invasive procedure performed in the interventional radiology department by specially trained staff, but understanding the procedure is useful for anyone educating patients or providing pre- and post-procedure care. Sedatives and/or painkillers will be administered. During fluoroscopy, a catheter is typically inserted into the right jugular vein and advanced down the superior vena cava into the right or middle hepatic vein. There, the contrast is used to identify the internal hepatic circulation. The TIPS needle is then inserted through the hepatic vein catheter into the portal vein. A stent is placed, connecting two veins to create a shunt, which reduces portal pressure.
If esophageal or gastric varices require embolization, coils, plugs, or sclerosing agents may be used. Throughout the procedure, the patient is monitored for cardiac arrhythmias.
AND
After the procedure (Lippincott Procedures, 2023)
Follow facility protocols and post-procedure recommendations, which may include:
- Overnight admission to the intensive care unit.
- Place the patient on the back of the bed for 4 hours with the head of the bed elevated at an angle of 30 to 45 degrees.
- Monitor vital signs, mental status, and access site (for bleeding or hematoma) every 15 minutes for the first hour, every 30 minutes for 2 hours, and hourly thereafter for 2 hours.
- Do strict intake and excretion as well as the patient’s daily weight.
- Get lab tests: complete blood count, coagulation panel, and liver and kidney function tests.
- Watch for signs of stomach bleeding.
- Watch for signs of encephalopathy.
- Measure your abdominal circumference.
- Limit your fluid and protein intake.
AND
Bajaj, J. S., Sanyal, A. J. & Collares, F. B. (2023, March 8). Overview of percutaneous intrahepatic portosystemic shunts (TIPS). Current. https://www.uptodate.com/contents/overview-of-transjugular-intrahepatic-portosystemic-shunts-tipsAND
AND
Lippincott Procedures (2023, May 22). Transjugular intrahepatic placement of a portosystemic shunt, assisted. . https://procedures.lww.com/lnp/view.do?pId=7136266&hits=portosystemic,intrahepatic,valve,shunts,transjugular
 Â
AND
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education12 months ago
Education12 months agoAI for teachers – Nursing Education Network






