Global Health
Understanding Diagnostics and Antibody Testing for COVID-19

Lack of access, insufficient supplies, and inconsistent or inaccurate results mean that testing for SARS-CoV-2, the virus that causes COVID-19, stays highly controversial and confusing. Here’s a summary of key concepts based on the evidence we currently have.
Terminology (Mahutte, 2019)
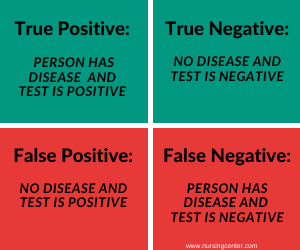 There are several terms you want to know that help describe the accuracy of a test, or its ability to measure what it was designed to measure.
There are several terms you want to know that help describe the accuracy of a test, or its ability to measure what it was designed to measure.
- is the probability that the test end in a sick person might be positive; high sensitivity allows sick patients to be missed and reduces the chance of false negative results.
- is the probability that a healthy person could have a negative test result; high specificity rarely gives a positive end in patients who aren’t sick and reduces the chance of false positive results.
The ideal test might be each highly sensitive and specific, with only a few false positives and false negatives. In addition, the predictive value of a test is the proportion of positive and negative results that could be expected based on the prevalence of the disease within the population. For example, a patient with a positive test result’s more more likely to have the disease if she or he lives in an area or population with a high prevalence of the disease.
Diagnostic test
A diagnostic test will indicate whether an individual has an lively SARS-CoV-2 infection. There are two varieties of tests available – molecular and antigen.
(U.S. Food and Drug Administration [FDA](2020a)
- Molecular tests detect the presence of the virus’s genetic material. Examples include:
- Nucleic acid amplification test (NAAT)
- Reverse transcription polymerase chain response (RT-PCR) test
- Sample sources:
- Nasopharyngeal swab (preferred)
- Pharyngeal swab
- Blood sample
- Stool sample
- The test is sort of sensitive and specific, but laboratory evaluation is time consuming.
- Positive results are typically verified by a confirmatory test.
- Negative results could also be unreliable for several reasons:
- Date of sample collection; peak viral shedding is unknown and the virus may not begin replicating for several days after initial exposure, so a sample collected too early may not detect the virus (false negative result).
- Incorrect sampling procedure.
- Incorrect materials; the swab ought to be product of Dacron or polyester material and placed in a viral transport medium.
- Delays in delivering the sample to the laboratory.
(FDA, 2020a)
- Antigen tests detect the presence of viral proteins and are utilized in acute or early infections since the antigen is detected when the virus is actively replicating.
- These tests, referred to as , aren’t as sensitive as molecular tests.
- Positive results are highly accurate.
- Negative results don’t rule out infection and will require confirmation by molecular testing before deciding on treatment.
- Based on similar RDT studies for influenza, sensitivity may range from 34% to 80%.
- More than 50% of COVID-19 patients could also be missed
- False positive results can occur if tests detect other coronaviruses, akin to those who cause the common cold.
- Factors affecting test reliability include (WHO, 2020):
- Time since onset of disease
- Virus concentration within the sample
- Quality of the sample taken
- How the specimen is processed
- Accuracy of reagent formulation in test kits
- Advantages
- Rapid results inside minutes; if sufficient virus concentration is detected, it binds to antibodies on the test strip and changes color inside half-hour.
- They could be produced more cheaply than PCR tests.
- Due to its easy design, it could possibly be scaled to check thousands and thousands of individuals per day.
- Sample sources:
- Nasopharyngeal swab
- Nasal swab
- Although the Food and Drug Administration (FDA) recently issued an Emergency Use Authorization (EUA) for an antigen test for COVID-19 (FDA, 2020b), based on current evidence, the WHO recommends that these tests be used only in research settings.
Antibody test
An antibody test will show whether an individual has had an infection, even in the event that they haven’t any symptoms.
- It doesn’t indicate whether an individual is currently infected. It mustn’t be used to diagnose COVID-19 infection.
- Detects antibodies called immunoglobulins:
- – the body produces them at the start of the acute phase of infection; these antibodies last for about 2 weeks, after which their levels decline.
- – the body produces them more slowly, inside 2–3 weeks after the initial infection, but their effects can last for months or years.
- – inhibit virus replication; their presence correlates with immunity.
- The antibody response will rely upon several aspects (WHO, 2020):
- Age
- Nutritional status
- Severity of the disease
- Immunosuppressive drugs
- Immune-weakening conditions akin to HIV
- Immunity based on SARS-CoV-2 antibody detection is just not certain at the moment, but these tests offer some public health advantages:
- Help determine the speed of infection in a population, potential herd immunity, and case fatality rate (Centers for Disease Control and Prevention (CDC, 2020a).
- To help discover individuals who’ve been infected with the SARS-CoV-2 virus and will now be eligible to donate convalescent plasma (CDC, 2020a).
- May support vaccine development (WHO, 2020).
- Different false positive and false negative rates.
- The CDC (2020a) recently stated that serologic tests could also be incorrect “up to half the time” and mustn’t be used to make decisions about return-to-school or workplace policies.
-
- Performed on a blood sample and sent to a laboratory for evaluation
- Detects IgG, IgM individually or combined as a complete antibody
- The results are more accurate but require trained laboratory personnel and specialized equipment.
- (World Health Organization, 2020):
- Detect IgG or IgG and IgM or total antibodies
- Results can be found inside minutes.
- Many of those tests haven’t been verified.
- Performed on the next samples:
- Serum, plasma, and whole blood, which could be obtained by finger prick quite than by intravenous catheterization
- Saliva, sputum or throat swab
- Determination of the power of antibodies to forestall viral infections in vitro.
- Research outside of the research setting is currently authorized by the FDA.
Who should get tested?
The CDC (2020b) identified individuals who ought to be offered priority testing.
- Symptoms of hospitalized patients
- Symptoms of healthcare staff, staff in collective housing and rescuers
- Residents of long-term care facilities or other collective housing, including prisons and shelters, symptoms
- Symptoms of potential COVID-19 infection, including fever, cough, shortness of breath, chills, muscle aches, latest lack of taste or smell, vomiting or diarrhea, and/or sore throat.
- Symptomatic individuals prioritized by health departments or medical professionals for any reason, including but not limited to: public health monitoring, sentinel surveillance, or screening of other asymptomatic individuals consistent with state and native plans.
How to enhance test reliability (CDC, 2020a)
To minimize false positive results and optimize the positive predictive value (95%), physicians and healthcare organizations should consider the next:
- Choose tests with high specificity (99.5% or higher)
- Test populations with a high prevalence or high pre-test probability of antibodies (e.g., individuals with a history of COVID-19 symptoms or who’ve had contact with areas with an outbreak).
- Apply a testing algorithm by which individuals who initially test positive are tested with a second, different test.
In an interview with Betsy Todd, MPH, RN, a nurse epidemiologist and clinical editor for Ms. Todd, she really useful searching for out tests offered by hospitals or public health facilities, since larger institutions usually tend to do the correct vetting to pick the perfect tests. For more information on COVID-19 testing, take heed to the total podcast with Ms. Todd.
What are your experiences with COVID-19 testing? Share them within the comments below.
Centers for Disease Control and Prevention (2020a). Evaluation and testing of people for coronavirus disease 2019 (COVID-19) [Interim Guidance for Healthcare Professionals]. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html
Food and Drug Administration (2020b). Frequently asked questions on SARS-CoV-2 testing. https://www.fda.gov/medical-devices/emergency-situations-medical-devices/faqs-testing-sars-cov-2
Centers for Disease Control and Prevention (2020a). COVID-19 testing. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html
Food and Drug Administration (2020b). Coronavirus (COVID-19) Update: FDA Authorizes First Antigen Test to Help Rapidly Detect the Virus That Causes COVID-19 in Patients. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-first-antigen-test-help-rapid-detection-virus-causes
Mahutte, NG, and Duleba, AJ (2019). Evaluation of diagnostic tests. UpToDate. https://www.uptodate.com/contents/diagnostic-tests-evaluation
World Health Organization (2020). Advice on using point-of-care immunodiagnostic tests for COVID-19, Scientific Brief. https://www.who.int/news-room/commentaries/detail/advice-on-the-use-of-point-of-care-immunodiagnostic-tests-for-covid-19
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education11 months ago
Education11 months agoAI for teachers – Nursing Education Network






