Global Health
T3 vs T4: What’s the Difference?

Thyroxine (T4) and three,5,3′-triiodothyronine (T3) are necessary hormones produced by the thyroid gland which can be essential for brain and physical development in infants and for metabolic activity in adults (Brent, 2022). Thyroid hormones also play a job in the conventional functioning of nearly every organ system, including the brain, heart, liver, and muscles. If left unregulated, thyroid hormone imbalances can result in life-threatening conditions corresponding to myxoid coma (dangerously low levels of thyroid hormone) and thyroid storm (excessive levels of thyroid hormone). Healthcare providers should know learn how to monitor these hormones to stop emergencies and improve outcomes.
Let’s take a more in-depth have a look at thyroid hormone production.
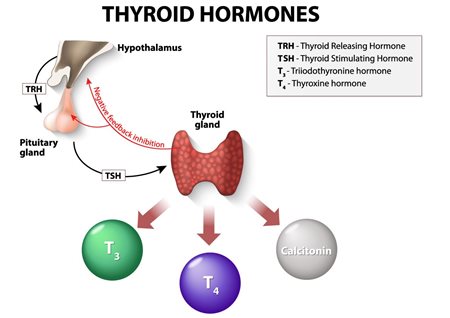
The thyroid gland, situated within the front of the neck, is made up of two kinds of cells: follicular cells, which produce T3 and T4, and parafollicular cells, which produce and secrete thyrocalcitonin (also called calcitonin). The thyroid gland takes iodine from our food plan, combines it with the amino acid tyrosine, and converts it into T3 (containing three atoms of iodine) and T4 (containing 4 atoms of iodine). T4 is produced exclusively by the thyroid gland at a rate of 80 to 100 mcg per day (Ross, 2024). About 80% of T3 is created by removing one atom of iodine from T4, a process called deiodination. This occurs primarily within the liver and kidneys, but T3 can be produced in some, if not all, tissues. Factors that inhibit the conversion of T4 to T3 include stress, fasting, beta-blockers, amiodarone, corticosteroids, iodinated contrast agents, and propylthiouracil (PTU). The thyroid gland synthesizes and stores bulk amounts of T3 and T4 within the protein thyroglobulin situated within the colloid space.
The production of T3 and T4 is regulated by thyroid-stimulating hormone (TSH) secreted by the pituitary gland, which in turn is regulated by thyroliberin-releasing hormone (TRH) secreted by the hypothalamus. This process works like a negative feedback loop. When T3 and T4 levels fall below normal, the pituitary gland produces TSH, stimulating the thyroid gland to supply more hormones and lift their levels within the blood. When levels rise, the pituitary gland reduces TSH production.
Thyroid hormones are released into the bloodstream and transported throughout the body. Most of them are certain to plasma proteins, while a smaller portion circulates as free hormones that enter cells and trigger metabolism. More than 99% of serum T4 and T3 are certain to serum proteins corresponding to thyroxine binding globulin (TBG), transthyretin (TTR), albumin, and lipoproteins. A minimal amount, roughly 0.02%, of serum T4 and 0.5% of serum T3 are free or unbound. It is the concentrations of free T3 and T4 within the blood which can be liable for biological activity and can be found for uptake by tissues (Ross, 2024). Binding proteins keep serum free T3 and T4 inside strict limits while ensuring that these hormones can be found to tissues when needed, thus acting as each storage and buffering systems. For example, if the thyroid gland stops secreting hormones, the hormones stored in serum will help delay the onset of hypothyroidism. T3 and T4 are rapidly released from the binding proteins and might turn into available almost immediately. Conversely, binding proteins also protect tissues from sudden increases in thyroid secretion or extrathyroidal T3 production.
What role do these hormones play in assessing thyroid function?
Thyroid function is assessed by a number of of the next tests:
-
- The typical range is 4.5 to five.0 mU/L, but normal values may vary between laboratories* (Ross, 2023).
- As mentioned earlier, very small changes in serum free T4 concentration stimulate very large changes in TSH concentration.
- High TSH levels indicate poor thyroid function or hypothyroidism. If the thyroid gland just isn’t producing enough hormone, the pituitary gland continues to supply and release TSH into the blood.
- A low TSH level normally indicates an overactive thyroid gland that produces an excessive amount of thyroid hormone, also generally known as hyperthyroidism. The pituitary gland then stops producing and releasing TSH into the blood.
-
- The typical range is 4.6 to 11.2 mcg/dL (60 to 145 mmol/L), but normal values may vary by laboratory* (Ross, 2023).
- Measures certain and unbound (free) T4.
- High serum T4 levels may indicate hyperthyroidism
- Low serum T4 levels may indicate hypothyroidism
- However, high or low levels may not indicate an issue. For example, in the event you are pregnant or taking oral contraceptives, your levels will probably be higher. Critical illness, corticosteroids, and medications for asthma, arthritis, and other health problems can lower T4 levels. These medications can change the quantity of binding proteins and subsequently may not accurately reflect T4 levels.
-
- A high T3 level will help confirm a diagnosis of hyperthyroidism if the T4 level is normal.
- The normal range varies more between laboratories than the full T4 level.
- The typical range is 75 to 195 ng/dL (1.1 to three nmol/L)* (Ross, 2023).
-
- Non-protein certain T4 measurements
- A low level of free T4 will indicate hypothyroidism.
- A high level of free T4 will indicate hyperthyroidism.
- It may provide a greater indicator of T4 levels since it just isn’t depending on binding proteins.
- The normal range varies depending on the methodology used.*
-
- Indirect measurement of thyroid hormone binding capability in serum.
- The normal range varies by laboratory.*
-
- It is derived from T4 and THBI and indicates how much free T4 is present in comparison with certain T4.
- FT4I will help determine if high T4 levels are brought on by an abnormal amount of TBG.
- The normal range varies by laboratory.*
*Check your institution’s standard laboratory ranges.
Thyroid dysfunction screening
Thyroid function tests (TFTs) are used to check thyroid activity, diagnose conditions corresponding to hyperthyroidism, Graves’ disease, hypothyroidism, Hashimoto’s disease, thyroid nodules, and thyroid cancer, and monitor thyroid substitute therapy and treatment for hyperthyroidism. Some physicians test all patients for TSH and free T4, but this might be expensive. In the outpatient setting, many providers use strategies corresponding to the next to scale back unnecessary laboratory testing (Ross, 2023):
- If TSH levels are normal, further testing just isn’t mandatory.
- If TSH levels are high, free T4 levels must be tested to find out the degree of hypothyroidism.
- If TSH levels are low, free T4 and T3 must be tested to find out the degree of hyperthyroidism.
- If pituitary or hypothalamic disease is suspected, serum TSH and free T4 levels must be measured.
- If TSH is normal however the patient has symptoms of thyroid dysfunction, serum free T4 concentration must be measured.
In patients with primary hypothyroidism who’re taking levothyroxine substitute therapy, serum TSH alone might be monitored (Ross, 2023). However, in patients with secondary hypothyroidism because of pituitary or hypothalamic disease with impaired TSH release, serum free T4 must be used to regulate thyroid hormone doses.
Monitoring patients with hyperthyroidism includes periodic clinical evaluations, serum free T4 levels, and total T3 levels. Treatment with antithyroid drugs, radioiodine, or surgery will affect serum TSH levels for several weeks to months. Once the condition has stabilized, TSH alone might be used to find out the effectiveness of treatment.
Assessment of thyroid function within the hospital setting just isn’t advisable unless there may be a powerful suspicion of thyroid disease, because changes in thyroid hormones, binding proteins, and TSH levels can occur in serious nonthyroid conditions (Ross, 2023). If thyroid disease is suspected, each serum TSH and free T4 or total T4 are needed to evaluate thyroid function in hospitalized patients.
Clinical presentation
Symptoms of hypothyroidism may include:
- Overall energy loss
- Slowed metabolism
- Weight gain
- Bradycardia
- Dry skin and hair
- Constipation
- Cold intolerance
- Swollen skin
- Hair loss
- Altered cognition
- Hyporeflexia
- Irregular periods/infertility in women
- Stunted growth in children
Symptoms of hyperthyroidism may include:
- Hot flashes, sweating
- Tachycardia
- Anxiety, nervousness
- Weight loss
- Hair loss
- Difficulty falling asleep, anxiety
- Hand shaking
- Weakness
- Diarrhea
- Emotional instability, irritability or fatigue
- I prefer
- Moist, sweaty skin
- Exophthalmos, drooping eyelid
In addition to those laboratory tests, physicians should at all times conduct a radical medical history, assess their clinical status, and reconcile all medications they’re taking when evaluating patients for thyroid disease.
Bibliography:
Brent, GA (2022, April 27). Thyroid hormone motion.. https://www.uptodate.com/contents/thyroid-hormone-action
Ross, D.S. (2024, January 9). Thyroid hormone synthesis and physiology. https://www.uptodate.com/contents/synteza-hormonów-thyroid-and-physiology
Ross, D.S. (2023, December 6). Laboratory assessment of thyroid function. https://www.uptodate.com/contents/laboratory-assessment-of-thyroid-function
.png.aspx)
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education12 months ago
Education12 months agoAI for teachers – Nursing Education Network






