Global Health
Is there a link between COVID-19 and the chance of stroke?
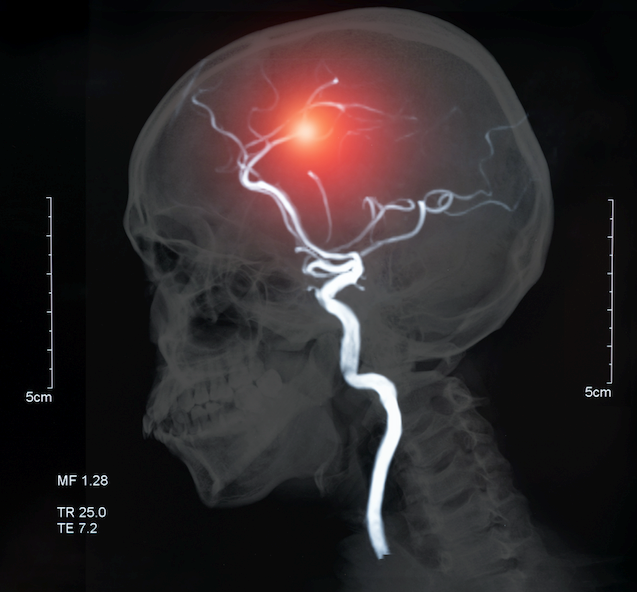
In a previous blog, we discussed how SARS-CoV-2, the virus that causes the coronavirus disease COVID-19, can trigger a cytokine storm resulting in inflammation and a hypercoagulable state, each of which put a patient at high risk of stroke. Healthcare providers have observed a disproportionately higher incidence of heart attacks amongst patients with Covid-19 in comparison with patients without the disease. Scientists are currently investigating whether there’s a link between COVID-19 and the chance of stroke.
In March this 12 months, Belani et al. (2020) assessed this relationship in a retrospective case-control study, collecting data from six hospitals. The aim of the study was to find out whether COVID-19 infection is related to an increased incidence of stroke and to evaluate whether it’s an independent risk factor for infarction when controlling for conventional vascular risk aspects (Belani et al., 2020). A cohort of 123 patients was enrolled within the study, and patients with acute ischemic stroke (occlusion of small or large vessels) were matched with patients without stroke (control group) in line with age, sex, and major vascular risk aspects, including hypertension, coronary artery disease, type 2 diabetes, atrial fibrillation, congestive heart failure, dyslipidemia, current or former smoking, evidence of previous stroke and body mass index (chubby or obese).
Belani et al. (2020) found that 19 of 41 patients (46.3%) with acute ischemic stroke had confirmed COVID-19 infection compared with 15 of 82 patients (18.3%) within the control group. After adjusting for age, sex, and major vascular risk aspects, the next were found:
- COVID-19 was an independent risk factor for acute ischemic stroke.
- Patients infected with COVID-19 have a significantly higher incidence of acute ischemic stroke in comparison with people without infection.
- COVID-19 infection is related to increased morbidity and mortality in comparison with previously documented infection outcomes.
- In patients with severe COVID-19, the incidence of heart problems was thrice higher than in individuals with mild or moderate disease.
In general, infections can result in systemic inflammation, platelet aggregation, and hypercoagulability, and lots of previous studies have associated recent infection with an increased short-term risk of ischemic stroke (Cowan et al., 2018). An evaluation of 727 cases of ischemic stroke by Cowan et al. (2018) found that 6.1% of patients had a hospital-acquired infection and 23.8% had an outpatient infection within the 90 days before stroke (Cowan et al., 2018). One of probably the most common infections preceding strokes was pneumonia/respiratory tract infection (15%) (Cowan et al., 2018). Hospital-acquired infection was a stronger trigger for stroke compared with outpatient infections, and the chance of stroke was highest immediately after infection (Cowan et al., 2018).
Mao et al. (2020) found that SARS-CoV-2 can infect the nervous system and skeletal muscles, and severe infection could cause further neurological damage, including acute cerebrovascular disease and decreased consciousness. Based on their research, Avula et al. (2020) suspect that increased levels of C-reactive protein (CRP), a marker of inflammation within the blood, and D-dimer (a marker of coagulation), may play a task within the pathophysiology of stroke in COVID-19 patients. Additionally, COVID-19 patients are at increased risk of medical complications akin to atrial arrhythmias, myocardial infarction, heart failure, myocarditis, and venous thrombosis, leading to greater susceptibility to acute ischemic events (Merkler et al., 2020).
Klok et al. (2020) assessed the composite consequence of symptomatic acute pulmonary embolism (PE), deep vein thrombosis, ischemic stroke, myocardial infarction, or systemic arterial embolism in 184 patients with Covid-19 pneumonia admitted to the ICU. The cumulative incidence of composite outcomes was 31%, with probably the most common complication being PE (Klok et al., 2020). Age and coagulopathy (prothrombin time greater than 3 seconds or activated partial thromboplastin time greater than 5 seconds) were independent predictors of thrombotic complications (Klok et al., 2020).
To reduce the incidence of acute ischemic stroke, the next strategies are advisable:
- Patients with COVID-19 needs to be evaluated early for acute neurological changes, and for patients suspected of stroke, investigation needs to be initiated immediately to cut back morbidity and mortality (Belini et al., 2020).
- In the case of patients with Covid-19 admitted to the ICU, it’s crucial to be sure that pharmacological thrombosis prophylaxis is implemented (Klok et al., 2020).
- Patients who develop a nosocomial infection may profit from preventive therapies for heart problems (antiplatelet agents and statins) (Cowan et al., 2018).
Increasing evidence confirms the link between Covid-19 infection and the occurrence of stroke. Although clinical practice doesn’t change significantly based on these findings, health care professionals should maintain an increased awareness of this risk.
Avula, A., Nalleballe, K., Narula, N., Sapozhnikov, S., Dandu, V., Toom, S., Glaser, A., and Elsayegh, D. (2020). COVID-19 presenting with stroke. , , 115-119. https://doi.org/10.1016/j.bbi.2020.04.077
Belani, P., Schefflein, J., Kihira, S., Rigney, B., Delman, B. N., Mahmoudi, K., Mocca, J., Majidi,., Yeckley, J., Arrarwal, A., Lefton, D. and Doshi, A. H. (2020). COVID-19 is an independent risk factor for acute ischemic stroke. . https://doi.org/10.3174/ajnr.A6650
Cowan, L. T., Lutsey, P. L., Pankow, J. S., Matsushita, K., Ishigami, J., and Lakshminarayan, K. (2018). Nosocomial and outpatient infection as a trigger for heart problems: the ARIC study. (22), 1-15. https://doi.org/10.1161/JAHA.118.009683
Klok, F.A., Kruip, M.J., van der Meer, N.J.M., Arbous, M.S., Gommers, DAMPJ, Kant, K.M., Kaptein, F.H.J., van Paassen, J., Stals, M.A.M., Huisman, M.V., and Endeman, H. (2020 ). Incidence of thrombotic complications in critically in poor health ICU patients with Covid-19. Thrombosis research. https://doi.org/10.1016/j.thromres.2020.04.013 .
Mao, L., Jin, H., Wang, M., Hu, Y., Chen, S., He, Q., Chang, J., Hong, C., Zhou, Y., Wang, D., Miao, X., Li, Y., and Hu, B. (2020). Neurological symptoms in hospitalized patients with coronavirus disease 2019 in Wuhan, China. 77(6):683-690. https://doi.org/10.1001/jamaneurol.2020.1127
Zayet, S., Klopfenstein, T., Kovacs, R. Stancescu, S., and Hagenkotter, B. (2020). Acute stroke with multiple infarcts and COVID-19, France, 2020. (9). https://wwwnc.cdc.gov/eid/article/26/9/20-1791_article
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education12 months ago
Education12 months agoAI for teachers – Nursing Education Network






