Global Health
Interpretation of liver enzymes and liver function tests
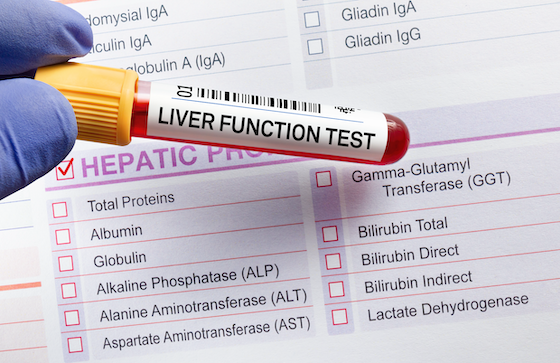
Liver enzymes and liver function tests (LFTs) are common laboratory tests performed in each primary care and acute care settings. They are used to evaluate liver function impairment, assess the extent of liver damage, and monitor the progression of liver disease and its response to treatment (Saiman, 2023). When screened with standard LFT panels, roughly 1 to 9% of asymptomatic patients have elevated liver enzyme levels (Malakouti, Kataria, Ali, & Schenker, 2017). These increases could also be short-lived and subside after a couple of weeks, but high levels can also signal acute injuries and chronic diseases.
Various reference ranges
When evaluating a patient’s blood test results, do not forget that reference ranges will vary from laboratory to laboratory. Additionally, certain ranges will differ between men and girls and will be higher in individuals with an increased body mass index (Lala, Zubair, & Minter, 2023).
| : occurs within the liver and other tissues; Elevated levels indicate liver damage and disease. | |
| Alanine aminotransferase (ALT) | Male: 29-33 units/liter (L) Female: 19–25 units/l |
| Aspartate aminotransferase (AST) | Males: 10–40 units/l Female: 9–32 units/l |
| Alkaline phosphatase (ALP) | Males: 45–115 units/l Female: 30–100 units/l |
| Gamma-glutamyl transpeptidase (GGT) | Male: 8–61 units/l Female: 5–36 units/l |
| 5′-nucleotidase (Friedman, 2022b) | 0.3–3.2 Bodanski units |
| Lactate dehydrogenase (LDH) (UpToDate, n.d.) | 80–225 units/l |
| indicates liver function, the power to provide protein, fibrinogen and vitamin K depending on coagulation aspects II (prothrombin), VII, IX and X. | |
| Total Protein (UpToDate, n.d.) | 5.5–9.0 g/100 ml (55–90 g/l) |
| Albumin | 3.5–5 g/100 ml (35–50 g/l) |
| Prothrombin time (PT) | 11.0–13.7 seconds |
| International Normalized Ratio (INR) (Shikdar, Vashisht and Bhattacharya, 2023) | Approximately 1.0 seconds |
| : bile pigment produced by the breakdown of blood proteins (hemoglobin) in aging red blood cells. The levels will indicate damage or obstruction of the bile ducts. | |
| Bilirubin, total (UpToDate, n.d.) | 0.3–1.0 mg/dl (5.1–17.1 mmol/l) |
| Direct, conjugated bilirubin (UpToDate, n.d.) | 0.1–0.3 mg/dl (1.7–5.1 mmol/l) |
| Indirect bilirubin, unconjugated (UpToDate, n.d.) | 0.2–0.7 mg/dl (3.4–12 mmol/l) |
General interpretation of liver enzymes and LFTs
Abnormal liver enzymes are assessed in three parts (Friedman, 2022a; Lala, Zubair, and Minter, 2023; Melendez-Rosado et al., 2018): pattern of elevation, degree of elevation, and clinical risk aspects.
Facade pattern
The elevation pattern provides information in regards to the source of injury (i.e., liver or bile ducts).
-
- Elevated AST and/or ALT levels out of proportion to ALP indicate liver tissue damage.
- Bilirubin could also be elevated; albumin and PT could also be abnormal.
- indicates acute or chronic viral hepatitis, steatohepatitis, acute Budd-Chiari syndrome, ischemic hepatitis, autoimmune disease, hemochromatosis, drugs/toxins, alpha1-antitrypsin deficiency, Wilson’s disease, or celiac disease.
- indicates alcohol-related liver disease, steatohepatitis, cirrhosis, or non-hepatic causes (hemolysis, myopathy, thyroid disease, exercise).
-
- Elevated ALP, GGT, and bilirubin levels out of proportion to AST and ALT indicate impaired bile production/excretion or biliary obstruction.
- Albumin and PT could also be abnormal.
- Hepatobiliary causes include biliary obstruction, primary biliary cirrhosis, primary sclerosing cholangitis, drug-induced, infiltrative liver disease (sarcoidosis, amyloidosis, lymphoma), cystic fibrosis, liver metastases, or cholestasis.
- Non-hepatic causes include bone disease, pregnancy, chronic kidney failure, lymphoma, congestive heart failure, infection, or inflammation.
-
- Increased ALP and AST/ALT levels
-
- Elevated bilirubin and normal ALP, AST and ALT levels
- Caused by increased production of bilirubin (pre-hepatic), decreased uptake or conjugation within the liver (hepatic), or decreased bile excretion and duct obstruction (ante-hepatic)
Degree of elevation
The degree of elevation will vary depending on the explanation for the injury.
- Limit: AST and/or ALT elevation is lower than 2 times the upper limit of normal (ULN).
- Mild: increase in AST and/or ALT 2 to five times the ULN.
- Moderate: AST and/or ALT elevation is 5 to fifteen times the ULN.
- Severe: AST and/or ALT increase greater than 15 times ULN.
- Massive: AST and/or ALT is bigger than 10,000 units/L.
Clinical risk aspects
- History of diabetes, hyperlipidemia, obesity, inflammatory bowel disease, celiac disease, thyroid disease, autoimmune disease, heart failure or acquired muscle disease.
- Family history of genetic liver disease comparable to Wilson’s disease, alpha-1-antitrypsin deficiency, or hereditary hemochromatosis.
- Social history, including travel, alcohol consumption and sexual behavior.
- Medicines comparable to acetaminophen, amiodarone, antibiotics (azithromycin, amoxicillin, nafcillin, rifampicin, tetracycline), antifungals (ketoconazole), antivirals (valaciclovir, ritonavir), antidepressants (fluoxetine), antipsychotics (risperidone), anticonvulsants (acid valproic acid, phenytoin), non-steroidal anti-inflammatory drugs (NSAIDs), methotrexate, anti-tuberculosis drugs (isoniazid, pyrazinamide, rifampicin), oral contraceptives, statins, anabolic steroids or herbal medicines.
Medical examination
When reviewing laboratory test results, all the time compare the outcomes to the patient’s physical examination when assessing for signs of chronic liver disease. Physical examination findings suggestive of liver disease include (Friedman, 2022a):
- ascites
- Hepatosplenomegaly
- Hepatic encephalopathy/neurological changes
- Jaundice
- Increased pressure within the jugular veins
- Muscular dystrophy
- Enlargement of the parotid gland
- Peripheral edema
- Itchy
- Testicular atrophy
Recognizing and understanding the various patterns of liver enzymes and LFTs together with a careful evaluation of the patient’s medical history, risk aspects, and physical examination will assist you to determine whether an elevation in these lab values is a cause for concern requiring additional diagnostics or a standard variant that could be watched over time. .
Friedman, L. S. (2022a, April 5). Approach to a patient with abnormal biochemical and liver function test results. .
https://www.uptodate.com/contents/podejście-do-pacjent-z-nieprawidłowych-testami-biochemiczne-i-funkcyjnemi-nątroby
Friedman, L. S. (2022b, July 28). Enzymatic measures of cholestasis (e.g. alkaline phosphatase, 5′-nucleotidase, gamma-glutamyl transpeptidase). . https://www.uptodate.com/contents/enzymatic-measures-of-cholestasis-eg-alkaline-fosfatase-5-nukleotidase-gamma-glutamyl-transpeptidase#H10
Lala, V., Zubair, M., & Minter, D. A. (2023, July 30). Liver function tests. Treasure Island (FL): StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK482489
Malakouti, M., Kataria, A., Ali, S. K., and Schenker, S. (2017). Elevated liver enzymes in asymptomatic patients – what should I do? , (4), 394–403. https://doi.org/10.14218/JCTH.2017.00027
Melendez-Rosado, J., Alsaad, A., Stancampiano, F. F., and Palmer, W. C. (2018). Abnormal liver enzymes. , (6), 497–507. https://doi.org/10.1097/SGA.0000000000000346
Saiman, Y. (2023, August). Laboratory tests of the liver and gallbladder. .
https://www.merckmanuals.com/professional/hepatic-and-biliary-disorders/testing-for-hepatic-and-biliary-disorders/laboratory-tests-of-the-liver-and-gallbladder
Shikdar, S., Vashisht, R., & Bhattacharya, P. (2023, May 1). International Normalized Ratio (INR). Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507707/
Current. (n.d.) Reference ranges for laboratory tests in adults. . https://www.uptodate.com/contents/laboratory-test-reference-ranges-in-adults
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education11 months ago
Education11 months agoAI for teachers – Nursing Education Network






