Global Health
Detection of tracheal deviation
Assessment of the trachea is a normal a part of every routine physical examination. It involves assessing the position of the trachea and detecting the deviation of the trachea from the midline. This is a serious clinical symptom, the reason for which must be identified and treated immediately.
What is tracheal deviation?
When the pressure within the chest cavity increases, the trachea may move to at least one side, normally the side where the pressure is lower or where there’s less lung volume. This abnormal positioning of the trachea may cause symptoms resembling coughing, difficulty respiratory, wheezing, and chest pain.
How to detect tracheal deviation during a physical examination? (Bickley et al., 2021)
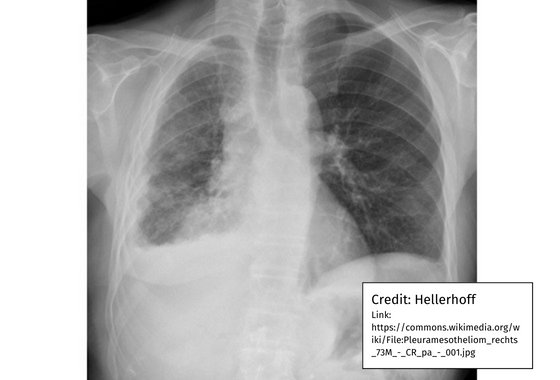
As you assess from head to toe and move right down to the neck, stop to envision the trachea for any deviation from the conventional midline position. The shift from the midline could also be subtle and difficult to detect on visual inspection. Then rigorously palpate for deviation by placing your finger along one side of the trachea and checking for space between it and the sternocleidomastoid muscle (SCM). Compare this to the opposite side of the trachea. The space must be symmetrical. Then listen for breath sounds over the trachea and listen for stridor, a high-pitched sound attributable to severe subglottic or tracheal obstruction. This is a respiratory emergency requiring immediate attention. If the patient doesn’t experience difficulty respiratory, a chest x-ray will help confirm the diagnosis and the necessity for further testing.
What causes tracheal deviation?
There are many causes of tracheal deviation, including:
- Neck injury, trauma, pneumothorax, bleeding
- Multinodular goiter
- Tumors, cancers, mediastinal lymphoma
- Pleural effusion
- Pneumonectomy
- Atelectasis
- Pleural fibrosis
- Pulmonary fibrosis
Treatment will rely upon severity and can concentrate on correcting the cause. Treatment includes respiratory exercises to enhance atelectasis, thoracocentesis to equalize pressure within the chest cavity, insertion of a chest tube to remove air or fluid from the pleural space, or surgery to remove a tumor or other obstructing structure.
Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bate’s guide to physical examination and interviewing (thirteenth ed.). Wolters Kluwer Health: Philadelphia.
Hinkle, J. (2021). Brunner and Suddarth’s textbook of medical-surgical nursing (fifteenth edition)vol ed.). Wolters Kluwer Health. https://wolterskluwer.vitalsource.com/books/9781975161057
.png.aspx)
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education12 months ago
Education12 months agoAI for teachers – Nursing Education Network






