Global Health
Contact tracing: a key element within the fight against COVID-19
Millions of Americans across the country are practicing social distancing and shelter-in-place orders, all united in an try and slow the spread of COVID-19. These efforts haven’t been in vain, as many cities are experiencing the long-awaited “flattening of the curve.” Leaders are currently developing plans to ease restrictions and reopen local economies, although exactly when that may occur has not been determined. The U.S. federal government has outlined a three-phase approach to Let’s reopen America it should NO begin until gating criteria are met and state authorities have implemented appropriate procedures that ensure they’re adequately prepared to stop further spread of the virus.
According to White House experts, the next gating criteria needs to be met before states begin to ease restrictions: 1. A downward trend in influenza-like illness (ILI) and COVID-like cases reported over a 14-day period; 2. A downward trend in documented COVID-19 cases over a 14-day period or a downward trend in positive tests (as a percentage of all tests) over a 14-day period; and three. Hospitals are capable of treat non-crisis patients along with an aggressive testing program for at-risk healthcare employees, including antibody testing (Whitehouse.gov, 2020). As of this writing, governors are expected to secure adequate personal protective equipment (PPE) and other medical supplies to address the numerous increase in demand, in addition to the rise in intensive care unit capability. Protecting those employed in critical industries, high-risk facilities, and mass transit stays a priority. States should encourage social distancing and recommend that folks wear masks in public. Continued surveillance is vital as any increase in recent COVID-19 cases should end in the reinstatement of previous restrictions to mitigate a second wave of infections.
Two key processes that should be established before entering Phase 1 are testing and get in touch with tracing. Testing has been controversial on account of the shortage of appropriate materials and chemicals, in addition to the dearth of reliability of the tests themselves. Once reliable testing is achieved, contact tracing and isolation should begin. Although this technique has not received as much media attention, the federal government has really helpful that states establish secure and efficient screening and testing sites for symptomatic individuals and get in touch with tracing of those that test positive for COVID-19 (Whitehouse.gov, 2020).
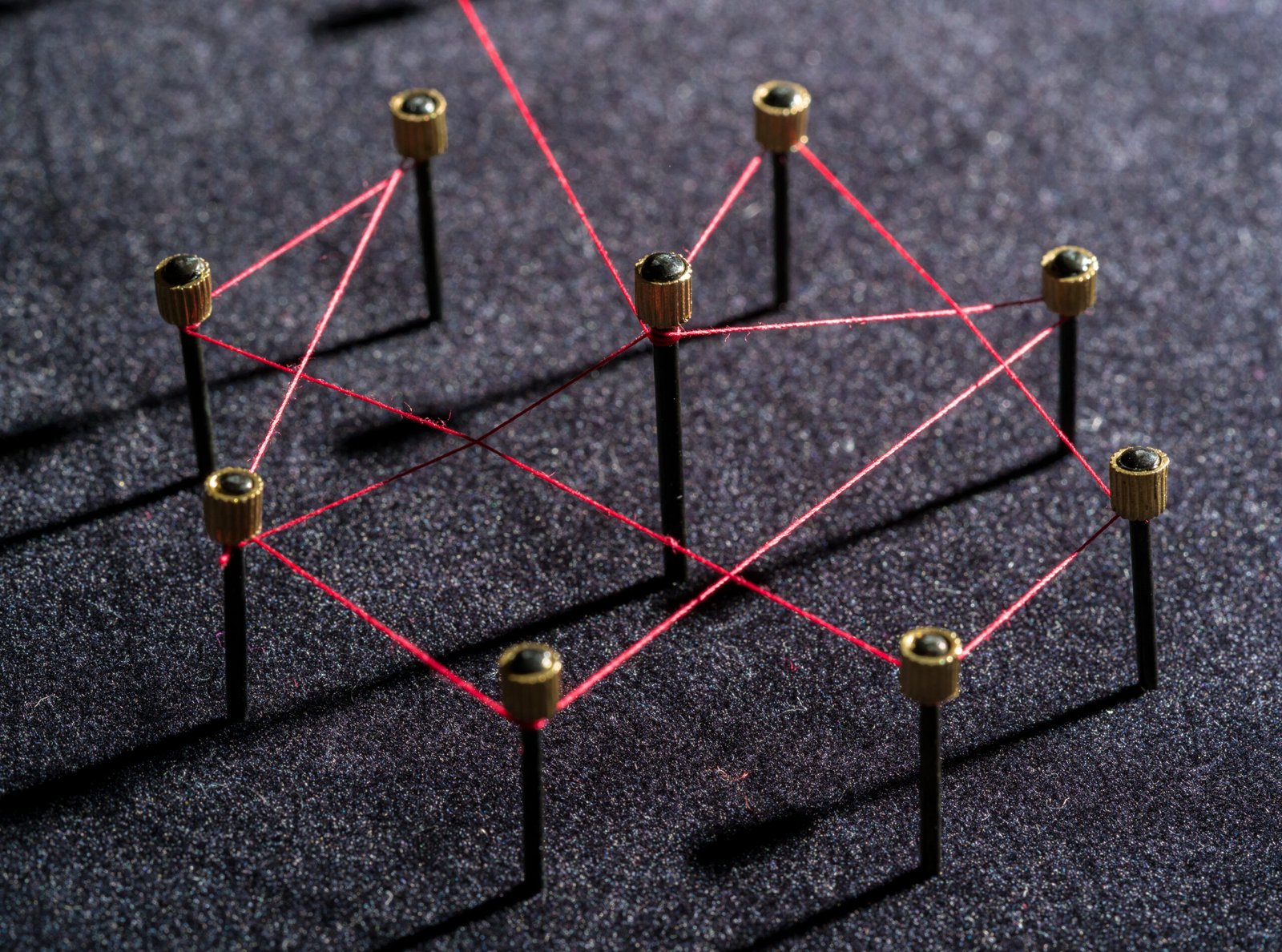
Contact tracing or contact investigation is a public health approach that has been used to contain pathogens including tuberculosis, polio, Ebola virus, and the primary severe acute respiratory syndrome (SARS) epidemic in 2003 (Cates et al., 2016; Shuaib et al., 2017). The goal of contact tracing is to discover, treat, and isolate current and potential cases of an infectious disease with a purpose to control and stop further human-to-human transmission. Countries akin to South Korea, China, Singapore, Germany, and New Zealand have used contact tracing with various degrees of success to hinder the spread of COVID-19 and reopen their economies.
- Identification: Once an individual is confirmed to have COVID-19 with a positive diagnostic test, ask them to self-quarantine at home in the event that they don’t require hospitalization. Interview them about their activities and folks they’ve had close contact with, akin to family, coworkers, friends, etc.
- Notification: A public health official will call each potential contact and notify them of the exposure. The contact might be asked to isolate at home and monitor for symptoms. The duration of quarantine may vary based on the extent of risk and duration of exposure.
- Isolation: Support secure, sustainable, and effective contact quarantine to stop further spread of the virus.
- Follow-up: Conduct follow-up interviews with all contacts to observe symptoms and check for infection if symptoms occur.
As previously mentioned, reliable testing is important for effective contact tracing. However, priority testing is being directed at hospitalized patients, symptomatic healthcare employees, patients in long-term care facilities, older adults, individuals with comorbidities with symptoms, symptomatic first responders, and symptomatic critical infrastructure employees (CDC, 2020b). Not every body with symptoms can or might be tested presently. Additionally, a high percentage of people that test positive for COVID-19 are asymptomatic and wouldn’t have access to testing. The inability to discover people who find themselves carrying the virus will hamper efforts to stop person-to-person transmission, making current stay-at-home orders an unlucky but critical necessity in lots of areas.
Contact tracing is labor-intensive and resource-intensive, requiring a big army of experienced individuals to coordinate and execute the hassle. In these circumstances, it isn’t feasible to conduct contact tracing interviews with lots of of hundreds of sick people, let alone their contacts. It will be done in smaller populations because the infection curve flattens and the number of recent cases declines. While several states have increased the variety of contact tracers, there isn’t a guarantee that a tracer will have the opportunity to trace down every contact. If they do, those contacts will not be following self-quarantine guidelines. Digital tools akin to mobile apps are getting used in other countries to increase and automate the method. However, here within the United States, privacy is a serious concern, and unless confidentiality is protected, this technology is unlikely to be adopted.
Experts warn that rushing to reopen the economy could backfire and send us right into a second wave of infections. Finding the fitting balance between easing restrictions and protecting essentially the most vulnerable might be difficult. For now, a cautious, measured approach is best.
Cates, J., Trieu, L., Proops, D., Ahuja, S. D. (2016). Contact investigations around patients with Mycobacterium tuberculosis with out a positive respiratory culture. 22(3), 275-282. DOI: 10.1097/PHH.00000000000000261
Centers for Disease Control and Prevention (2020a). Contact Tracing: Open America: Supporting States, Tribes, Localities, and Territories Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/php/open-america/contact-tracing.html
Centers for Disease Control and Prevention (2020b). Priorities for testing patients with suspected COVID-19 infection. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/downloads/priority-testing-patients.pdf
Shuaib, F. M., Musa, P. F., Muhammad, A., Musa, E., Nyanti, S., Mkanda, P., Mahoney, F., Corkum, M., Durojaiye, M., Nganda, G. W., Sani, S. U., Dieng, B., Banda, R., and Ali Pate, M. (2017). Containing Ebola and Polio in Resource-Scarce Settings Using Public Health Emergency Operations Center Principles and Practices. 23(1), 3 – 10. DOI: 10.1097/PHH.00000000000000447
Whitehouse.gov and Centers for Disease Control and Prevention (2020). Guidelines – Opening Up America Again. Downloaded from https://www.whitehouse.gov/openingamerica/#criteria
World Health Organization (2017). Contact tracing. Retrieved from https://www.who.int/news-room/qa-detail/contact-tracing
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being11 months ago
Well-Being11 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education11 months ago
Education11 months agoAI for teachers – Nursing Education Network






