Global Health
Calculation of cerebral perfusion pressure
Cerebral perfusion pressure (CPP) is the quantity of pressure needed to keep up blood flow to the brain. CPP is regulated by two balanced, opposing forces:
- Mean arterial pressure (MAP) is the driving force that pumps blood to the brain.
- Intracranial pressure (ICP) is the force that stops blood from leaking out of the skull.
Indications
CPP monitoring is helpful in guiding the treatment of patients with traumatic brain injury, low-grade subarachnoid hemorrhage, stroke, intracerebral hematoma, meningitis, acute liver failure, and hydrocephalus.
Formula
- Here is the patient information you may have:
Blood pressure: 130/73 ICP: 14 mm Hg
- Use the formula: CPP = MAP – 14
- Calculate MAP using the formula MAP = [SBP + 2(DBP)] ÷ 3
MAP = [130+2(73)] ÷ 3
MAP = (130+146) ÷ 3
MAP = 276 ÷ 3
MAP = 92 mmHg
- Substitute ICP and MAP into the CPP formula.
CPP = 92 – 14
CPP = 78 mmHg
Interpretation
- Brain Trauma Foundation guidelines recommend a CPP of 60–70 mmHg in patients with severe brain injury (Carney et al., 2019).
- Maintaining CPP throughout the goal range may prevent secondary injury as a result of hypoperfusion (e.g., ischemia) or hyperperfusion (e.g., increased edema).
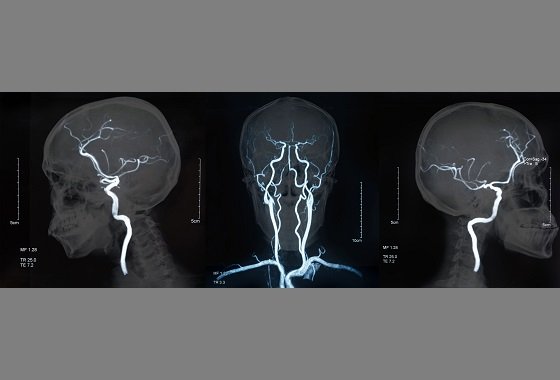
- Brain monitoring techniques corresponding to transcranial Doppler (TCD)/duplex ultrasound, arterial and arteriovenous oxygen differences (AVDO)2) and measurements of local tissue oxygenation provide complementary and detailed information that will help determine optimal CPP and ICP targets for individual patients.
Management principles
- To achieve adequate CPP, physicians must discover a balance between treating the explanation for the elevated ICP and appropriately treating the patient’s blood pressure.
- Even if CPP is inside the suitable range, ICP elevations greater than 20–25 mm Hg and/or hypotension must be treated promptly. Treatment of elevated ICP may include decompressive craniectomy, CSF drainage, hyperosmotic therapy, ventilation strategies, and sedation (Smith & Amin-Hanjani, 2024).
Carney, N., Totten, A. M., O’Reilly, C., Ullman, J. S., Hawryluk, G. W., Bell, M. J., Bratton, S. L., Chesnut, R., Harris, O. A., Kissoon, N., Rubiano, A. M., Shutter, L., Tasker, R. C., Vavilala, M. S., Wilberger, J., Wright, D. W., & Ghajar, J. (2019). Guidelines for the treatment of severe traumatic brain injury, fourth edition. , (1), 6–15. https://doi.org/10.1227/NEU.00000000000001432
Munakomi S, & Das JM. Monitoring intracranial pressure. (23 January 2024). In; 2024 January.https://www.ncbi.nlm.nih.gov/books/NBK542298/
Smith, ER and Amin-Hanjani, S. (2024, May 29). Evaluation and treatment of elevated intracranial pressure in adults. https://www.uptodate.com/contents/evaluation-and-treatment-of-intracranial-pressure-in-adults
.png.aspx)
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being11 months ago
Well-Being11 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being11 months ago
Well-Being11 months agoHow to get the standard of sleep for higher mental health
-

 Education11 months ago
Education11 months agoAI for teachers – Nursing Education Network






