Global Health
Acute Kidney Injury and Chronic Kidney Disease – What’s the Difference?

Kidney failure develops when the kidneys turn into unable to filter waste products from the blood adequately. It is brought on by a wide selection of diseases and medications which have acute or chronic effects on the kidney’s blood vessels, tubules, or glomeruli.
Acute kidney injury
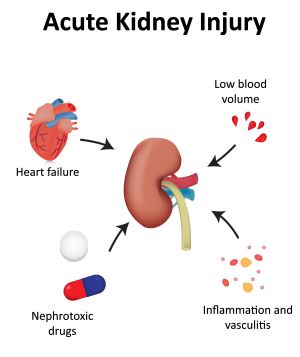 Acute kidney injury (AKI), formerly generally known as acute renal failure, is a sudden decline in glomerular filtration rate (GFR). This ends in increased serum creatinine (SCr), blood urea nitrogen (BUN), and electrolyte levels (Okusa and Rosner, 2023). Acute kidney injury is a spectrum of clinical conditions: it may possibly be rapidly reversible with prompt identification and treatment of the underlying cause, reminiscent of fluid substitute for dehydration or removal of nephrotoxin. On the opposite hand, life-threatening fluid overload or electrolyte abnormalities can occur, requiring urgent dialysis before the cause will be identified. Many cases of AKI occur in patients hospitalized for an unrelated acute illness.
Acute kidney injury (AKI), formerly generally known as acute renal failure, is a sudden decline in glomerular filtration rate (GFR). This ends in increased serum creatinine (SCr), blood urea nitrogen (BUN), and electrolyte levels (Okusa and Rosner, 2023). Acute kidney injury is a spectrum of clinical conditions: it may possibly be rapidly reversible with prompt identification and treatment of the underlying cause, reminiscent of fluid substitute for dehydration or removal of nephrotoxin. On the opposite hand, life-threatening fluid overload or electrolyte abnormalities can occur, requiring urgent dialysis before the cause will be identified. Many cases of AKI occur in patients hospitalized for an unrelated acute illness.
Chronic kidney disease
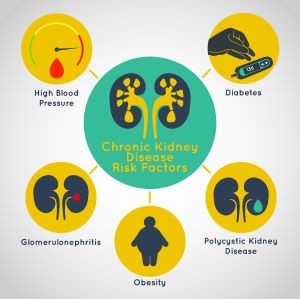 Chronic kidney disease (CKD) is defined because the presence of kidney damage or decreased GFR for greater than 3 months. Kidney damage is characterised by albuminuria, urine casts, imaging findings, or abnormal renal biopsy. CKD is brought on by long-term diseases reminiscent of diabetes or hypertension. Patients could have symptoms which can be directly related to decreased kidney function. These include malaise, nausea, decreased mental acuity, swelling, or decreased urine production. However, many patients haven’t any clinical symptoms. In these patients, kidney disease is detected by laboratory tests which can be performed during routine screening or as a part of the evaluation of an unrelated disease. The stages of CKD are a continuum and are
Chronic kidney disease (CKD) is defined because the presence of kidney damage or decreased GFR for greater than 3 months. Kidney damage is characterised by albuminuria, urine casts, imaging findings, or abnormal renal biopsy. CKD is brought on by long-term diseases reminiscent of diabetes or hypertension. Patients could have symptoms which can be directly related to decreased kidney function. These include malaise, nausea, decreased mental acuity, swelling, or decreased urine production. However, many patients haven’t any clinical symptoms. In these patients, kidney disease is detected by laboratory tests which can be performed during routine screening or as a part of the evaluation of an unrelated disease. The stages of CKD are a continuum and are
classified as follows (Kellum and Lemeire, 2012):
- Stage 1: Renal impairment with normal or increased GFR (>90 ml/min/1.73 m2)
- Stage 2: Mild reduction in GFR (60–89 ml/min/1.73 m2)
- Stage 3a: Moderate reduction in GFR (45–59 ml/min/1.73 m2)
- Stage 3b: Moderate reduction in GFR (30–44 ml/min/1.73 m2)
- Stage 4: Significant reduction in GFR (15–29 ml/min/1.73 m2)
- Stage 5: Renal failure (GFR < 15 ml/min/1.73 m2 or dialysis)
The table below shows the clinical features of AKI and CKD. However, presenting AKI and CKD as completely separate clinical entities is somewhat misleading. In recent years, CKD has been recognized as a significant risk factor for the event of recent AKI, and patients with CKD who develop AKI often don’t get well fully and experience accelerated deterioration of renal function (Ferenbach and Bonventure, 2016).
| Beginning | Sudden | Gradually (months or years) |
| Most common causes |
|
|
| Diagnosis* | One of the next:
|
One of the next, for a minimum of 3 months:
|
| Symptoms |
|
|
| Reversibility | Usually reversible | Irreversible, progressive |
| Management |
|
|
In summary, AKI develops suddenly because of this of acute kidney injury. It covers a spectrum of renal dysfunction from minor changes in markers of renal function to the necessity for renal substitute therapy (RRT). Treatment for AKI involves identifying and treating the underlying cause and minimizing complications. AKI is often reversible. In contrast, CKD develops step by step, over months or years, because of this of chronic diseases reminiscent of diabetes and hypertension. Patients are sometimes asymptomatic, and CKD is discovered incidentally during routine screening or diagnostics for unrelated conditions. Medical treatment can slow the progression of renal failure, but it surely is irreversible and ultimately results in the necessity for kidney transplantation or everlasting dialysis.
Ferenbach, D. A. and Bonventre, J. V. (2016, April). Acute kidney injury and chronic kidney disease: from the laboratory to the clinic.): S41-S48.
Kellum, JA, & Lameire, N. (2012, March). KDIGO clinical practice guidelines for acute kidney injury.
Levey, AS and Inker, LA (2024, May 1). Definition and stages of chronic kidney disease in adults. https://www.uptodate.com/contents/definition-and-staging-of-chronic-adult-kidney-disease
Okusa, MD and Rosner, MH (2023, November 7). Review of the treatment of acute kidney injury (AKI) in adults.https://www.uptodate.com/contents/overview-of-the-management-of-acute-kidney-injury-aki-in-adults
Rosenberg, M. (2022, November 10). Overview of the treatment of chronic kidney disease in adults. https://www.uptodate.com/contents/overview-of-the-management-of-chronic-kidney-disease-in-adults
National Institute for Health and Care Excellence. (2023, September 28). Acute kidney injury: prevention, detection, and treatment. https://www.nice.org.uk/guidance/ng148
.png.aspx)
-

 Well-Being1 year ago
Well-Being1 year ago5 books that may help at work at work
-

 Global Health1 year ago
Global Health1 year agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being1 year ago
Well-Being1 year agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being12 months ago
Well-Being12 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice10 months ago
Best Practice10 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being12 months ago
Well-Being12 months agoHow to get the standard of sleep for higher mental health
-

 Education11 months ago
Education11 months agoAI for teachers – Nursing Education Network






