Global Health
Is COVID-19 fueled by a cytokine storm?
SARS-CoV-2, the virus that causes COVID-19, continues to baffle even probably the most seasoned infectious disease experts. One troubling issue is the growing variety of young people between the ages of 20 and 60 who’re contracting COVID-19 and developing serious illness that requires intensive care. Even more troubling is that a few of these patients haven’t any known underlying condition that predisposes them to greater risk.
One phenomenon which will play a task in COVID-19 is cytokine release syndrome (CRS), also generally known as cytokine storm. CRS has been described as an acute systemic inflammatory syndrome or exaggerated immune response characterised by fever and multi-organ dysfunction (Porter & Maloney, 2019). It occurs in patients undergoing immune-based cancer treatments similar to chimeric antigen receptor (CAR) T-cell therapy and may also occur after treatment with a therapeutic antibody (i.e. blinatumomab) or haploidentical allogeneic hematopoietic cell transplantation. A CRS-like syndrome that develops after a severe viral infection is also known as a cytokine storm reasonably than CRS. Scientists hypothesize that some form of cytokine storm contributed to the high mortality related to previous viral epidemics, similar to the 1918 H1N1 Spanish flu, the 1957 H2N2 Asian flu, the 1968 H3N2 Hong Kong flu, the 2009 H1N1 pandemic flu, and the 1997–2014 avian influenza, which was attributable to several different H5N1, H7N9, and H10N8 strains (Liu, Zhou, & Yang, 2016).
Storm Pathology (Liu, Zhou, and Yang, 2016)
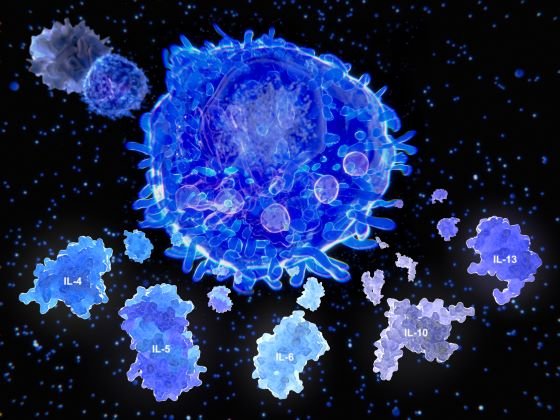
The pathology of cytokine storms shouldn’t be fully understood, but much has been learned about them. Viruses typically goal respiratory epithelial cells, which trigger a cytokine response. Pattern recognition receptors (PRRs) on immune cells recognize the virus and signal the discharge of proinflammatory cytokines, similar to interferon gamma (IFN-g), tumor necrosis aspects (TNF), interleukins (ILs), and chemokines (Liu, Zhou, & Yang, 2016). IFN-g prompts macrophages, which produce IL-6, TNF-α, and IL-10.
Macrophages are the first cells recruited to the alveolar space initially in response to viral infection. They increase cytokine production and attract additional immune cells to the affected area, similar to CD4 and CD8 T helper cells, which function to combat the virus. Additional PRR-related pathways are activated, including cyclooxygenase (COX)-2 and c-Jun N-terminal kinase (JNK). Once the virus is cleared, the immune pathways are turned off.
However, in a cytokine storm, this process doesn’t stop because it should. Inflammatory cytokines go into overdrive and may enter the bloodstream, causing systemic cytokine storms and ultimately multi-organ dysfunction. IL-6 has been implicated in vascular leakage, coagulation cascades, disseminated intravascular coagulation (DIC), and cardiomyopathy (Porter & Maloney, 2019). IFN-g may cause fever, chills, headache, dizziness, and fatigue, while TNF-α can result in fever, malaise, vascular leakage, cardiomyopathy, and lung damage. Genetics could also be one factor that might explain why some people develop only mild symptoms while other young, healthy patients change into very unwell.
Laboratory results
Early data from patients with severe COVID-19 show laboratory findings consistent with a cytokine storm, similar to elevated inflammatory markers (i.e., D-dimer, ferritin) and increased proinflammatory cytokines, that are related to critical and life-threatening disease (McIntosh, 2020). Mehta et al. (2020) state that patients with COVID-19 exhibit clinical features much like secondary hemophagocytic lymphohistiocytosis (sHLH), one other aggressive and fatal immune overreaction syndrome that is often attributable to viral infections and develops in some patients with sepsis. Symptoms include fever, cytopenias, high ferritin, and acute respiratory distress syndrome (ARDS) (Mehta et al., 2020). Physicians should consider screening patients with severe COVID-19 for markers of excessive inflammation, similar to increased ferritin, decreased platelet count, or ESR, to differentiate patients who might profit from immunosuppressive therapy (Mehta et al., 2020).
Potential Treatment Strategies
We don’t have a magic solution. It could take a minimum of a yr, and maybe even longer, before an efficient vaccine is developed, tested, and approved to be used against COVID-19. In the meantime, several immunomodulatory therapies have the potential to treat patients with infection who experience a cytokine storm:
- Corticosteroids: Although not typically advisable for the treatment of COVID-19-induced lung injury, immunosuppression with corticosteroids could also be useful in treating excess inflammation (Mehta et al., 2020).
- Selective cytokine blockade, e.g. anakinra or tocilizumab:
- Anakinra, a recombinant human IL-1 receptor antagonist currently used to treat rheumatoid arthritis, is currently undergoing clinical trials to scale back excessive inflammation and respiratory distress in patients with COVID-19.
- Tocilizumab, an IL-6 receptor blocker indicated for the treatment of CRS, has been approved in China for the treatment of COVID-19-induced pneumonia and elevated IL-6 levels (Mehta et al., 2020).
- Intravenous immunoglobulin:
- Concentrated globulin prepared from pooled human plasma has been used to treat SARS-CoV-1 (classical SARS) and the 2009 H1N1 influenza pandemic (Liu, Zhou, & Yang, 2016). Convalescent plasma from recovered COVID-19 patients is being investigated as a possible treatment.
- Janus kinase (JAK1/JAK2) inhibitors may impact inflammation and viral entry into cells in COVID-19 patients (Mehta et al., 2020).
The individual’s response to infection appears to be determined by each viral virulence and host resistance (Liu, Zhou, & Yang, 2016). Previous experience with viral epidemics has shown that immunomodulators together with antiviral drugs may be effective in treating severe disease. However, until randomized controlled trials are conducted to prove the efficacy of the therapies described above, clinicians should proceed to follow the most recent Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19) guidelines when providing care on the bedside.
Liu, Q., Zhou, Y. & Yang, Z. (2016). Severe influenza cytokine storm and development of immunomodulatory therapy. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4711683/
McIntosh, K. (2020). Coronavirus disease 2019 (COVID-19). . Retrieved from https://www.uptodate.com/contents/coronavirus-diseases-2019-covid-19
Mehta, P., McAuley, D. F., Brown, M., Sanchez, E. Tattersall, R. S., and Manson, J. (2020). COVID-19: consider cytokine storm syndromes and immunosuppression. . Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30628-0/full text
Porter, DL, and Maloney, DG (2019). Cytokine release syndrome (CRS). . Retrieved from https://www.uptodate.com/contents/cytokine-release-syndrome-crs?
Yuen, K., Ye, Z., Fung, S., Chan, C., & Jin, D. (2020). SARS-CoV-2 and COVID-19: key research questions. Cell & Biology. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074995/
-

 Well-Being11 months ago
Well-Being11 months ago5 books that may help at work at work
-

 Global Health12 months ago
Global Health12 months agoThe Global Fund opens up the potential of private sector investment – updates
-

 Well-Being12 months ago
Well-Being12 months agoFast and healthy advice on preparing meals for busy nurses
-

 Well-Being10 months ago
Well-Being10 months agoMaintenance of the nursing engine – each day nurse
-

 Best Practice9 months ago
Best Practice9 months agoSafety within the workplace as an ethical imperative in nursing
-

 Best Practice1 year ago
Best Practice1 year agoA cultural approach to the treatment of neonatal pain
-

 Well-Being10 months ago
Well-Being10 months agoHow to get the standard of sleep for higher mental health
-

 Education10 months ago
Education10 months agoAI for teachers – Nursing Education Network






